Stereotactic Body Radiotherapy (SBRT) is one of several ablative therapy options for the treatment of liver metastases. In order to ensure a sufficient local tumor control rate, the biologically equivalent dose (BED) should be at least 100 Gy (assuming an α/β ratio of 10). See for instance the DEGRO recommendations1.
Recently, we reported the first clinical treatment of this kind in our institute. All images shown on this page are taken either from this first patient or from preparatory phantom studies.
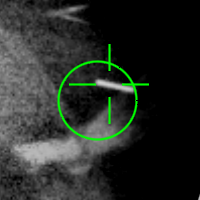
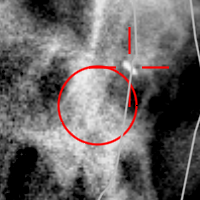
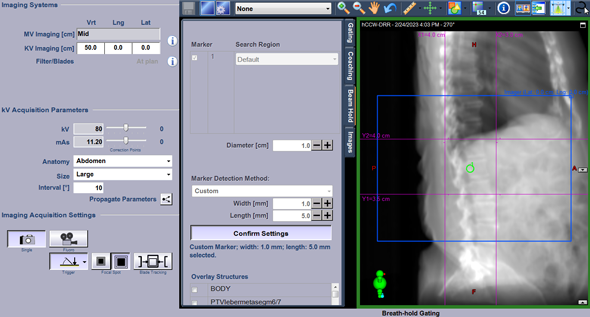
This series of kV images was acquired during the CCW half arc of the second fraction. Every 10° of Gantry angle, a kV image is triggered without interrupting the MV beam (which always comes from the right, orthogonal to the kV beam):
(kV marker tracking during MV treatment as seen by Offline Review. Circle diameter is 1 cm.)
Anticipated Challenges
The technical challenges when treating liver metastases stereotactically are at least twofold:
- Image contrast during IGRT procedures
- Motion
Lung metastases can easily be identified on CT and CBCT images, due to the large HU difference between the tumor and the surrounding lung tissue. In the liver however, the density difference is much smaller. While registered MR images are used to support target delineation in the planning phase, the daily treatement on a typical linac has no MR support. Therefore, the tumor is often not visible on the CBCT image. This is where fiducial markers come into play.
Tumor motion, mainly due to breathing, is another challenge. Two paths can be followed, depending on the capabilities of the patient:
- If the patient is capable of holding his breath for a certain amount of time, Deep Inspiration Breath Hold (DIBH) is the option of choice: the treatment is time efficient because the beam is always on2.
- If the patient is unable to hold his/her breath but breathing rate is stable, a 4D planning CT can be acquired and phase gating to a certain fraction of the breathing cycle (e.g., the exhale part) can be considered. An average CT generated from the chosen exhale phases is used for treatment planning. During treatment, a Gated CBCT of the same exhale phases is acquired and used for online matching.
The motion amplitude during the breathing cycle depends on the location of the tumor within the liver, and can be up to 4 cm and more.
It must be noted that external surrogate markers like the IR marker block do not always work as expected: unlike with the QUASAR Motion Platform (see sidebar) and its fixed 1:4 amplitude ratio, there is no simple mechanical translation between external motion and internal motion in the patient. One may observe day-to-day variations in tumor motion even if externally detected breathing motion is exactly the same.
This is why it is important to track deep-seated moving targets directly during the treatment.
Our First Patient: Marker Choice, Implantation, Imaging
For our first patient, we decided to use a single platinum marker of dimensions 0.5 x 5.0 mm. Platinum is preferred to gold because it produces less artefacts in MR.
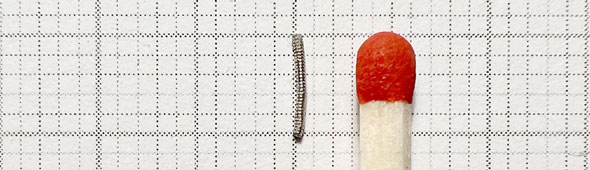
(The Visicoil platinum marker used in phantom studies.)
A specialist of our radiology department implanted the marker (needle: 21G, 15 cm length) with ultrasound guidance into the periphery of the tumor lesion, exactly as desired. This was preceded by some discussion about the ideal marker location and the required number of markers. Motion phantom studies on the TrueBeam with more than one marker and ABH (see sidebar) suggested that the automatic marker detection algorithm did not always distinguish correctly between the markers, and that it would be safer to use a single marker. On the other hand, there may be a certain risk of spreading tumor cells if the needle goes right into the center of the lesion. Therefore our choice.
One week after implantation, several MR studies were acquired. Only a moderate dark spot on the location of the marker appears on the MR image (MR contrast agent: 9 ml Primovist):
(Registered DIBH planning CT and MR images of our first patient.)
The MR studies were registered to our DIBH planning CT.
Since we did not know at this stage whether the patient would be able to hold her breath long enough for treatment, we also acquired a 4D-CT.
In the following animation, one can see that the marker moves in all three axes during a breathing cycle:
(4DCT with implanted platinum fiducial marker)
While the cranio-caudal amplitude is the largest with 1.2 cm, lateral and dorso-ventral movements are also visible. Both have an amplitude of 0.55 cm. This results in an overall amplitude of 1.43 cm between peak inhale and peak exhale.
As it turned out that DIBH treatment would be feasible, target delineation and planning proceeded on the DIBH-CT.
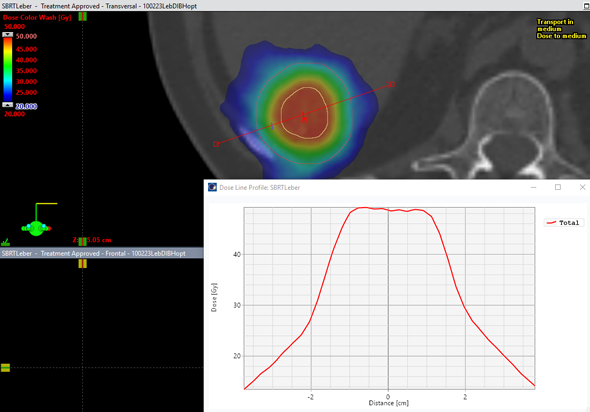
The GTV (volume: 6.9 cm3) was expanded to the PTV with an isotropic 1 cm margin (see the two structures in the next image).
Dose Planning
For our first patient, we chose a prescription of 5 x 6 Gy prescribed to the 60% isodose of the PTV. This gives a fraction dose of 10 Gy in the center of the lesion and a BED of 100 Gy.
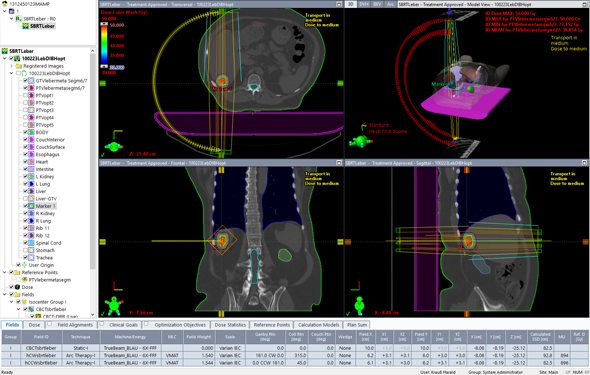
The treatment plan contained two 6FFF half arcs, optimized with the Eclipse Photon Optimizer 16.1 and calculated with Acuros XB 16.1.
The plan was then dosimetrically verified with Varian Portal Dosimetry, see the 2 % / 2 mm Gamma results for the hCW and hCCW arcs.
Treatment Preparation
The DIBH breathing curve which had been recorded on the RGSC System at the time of planning CT image acquisition was attached to the (gated) treatment plan. Lower and upper limits for the Varian Gating System were set to 1.65 - 2.15 cm, which means that the vertical excursion of the IR-marker block on the patient's belly must be within a 5 mm wide band in order to enable beam on.
On the TrueBeam, certain choices have to be made during the first session which cannot be prepared in ARIA: The CBCT imaging procedure for instance is set to Gated CBCT. A reconstruction slice thickness of 1 mm in not strictly necessary for a precise match result. However, with 1 mm the shape of the marker and its orientation in space can be resolved.
To the (VMAT) treatment arcs, triggered "During" kV images have to be added. We chose a trigger interval of 10° of Gantry angle. After switching off Blade Tracking, the kV blades can be closed to a small area around the marker:
With the specification of marker dimensions (width and length) the preparation is complete.
From this point, treatment proceeds similar to a conventional DIBH, but with added security: while the breathing curve is monitored continuously and the MV beam is held off as soon as the gate is left, every 10° a kV image appears on the screen with instant marker detection and either ABH (if selected) or at least a clear visual information whether treatment is still on track.
The possibility of marker tracking renders high dose ablative treatments a very safe procedure.
Notes
1 Florian Sterzing et al.: Stereotactic body radiotherapy for liver tumors: principles and practical guidelines of the DEGRO Working Group on Stereotactic Radiotherapy, Strahlenther. Onkol. 2014 Oct;190(10):872-81
2 If some treatment interruptions occur because the patient wishes to exhale, this is no problem. TrueBeam Motion Management will hold the beam immediately. It is more important that the patient can breath in repeatedly to the same depth, and then hold the plateau for a certain amount ot time. Training sessions on the CT (without imaging) are used to train the patient.