Introducing HyperArc
HyperArc™ is Varian's approach for standardized VMAT planning and treatment of multiple lesions in the brain, using a single isocenter. The set of treatment fields consist of one 360° full arc and up to three 180° half arcs with couch rotation. If the isocenter is inside the collision free "Patient Protection Zone", all arcs can be used, and the treatment sequence looks like this1:
(Virtual Dry Run in Eclipse. Note that the patient is the actual patient from the plan.)
While the angles of couch rotation are always 0°, 45°, 315° and 270° (Varian IEC scale), the collimator rotation is optimized during planning.
HyperArc Planning
HyperArc planning differs from normal VMAT planning in several ways:
- A special SRS immobilization system (Encompass™ from QFix) is required. In Eclipse, the Encompass Support is available as model, which is added to the planning CT instead of the normal couchtop model.
- Target structures should be defined as High Resolution Structures in Contouring, otherwise a warning will be issued.
- In Photon Optimizer (PO), the HyperArc-specific Stereotactic Radiosurgery Normal Tissue Objective Auto (SRS NTO) is activated instead of the standard NTOs.
- All targets get a lower objective at 100% volume and the dose level as set in the HyperArc dialog box (see below). No upper objective is automatically generated2.
- If no upper objective exists, it is possible to use the Automatic Lower Dose Objective (ALDO). This automates the attainment of equal relative coverage of 98% among all targets. In other words, the target DVH curves are bundled at 98%, by modifying the user-given target priorities during optimization.
- Structure Resolution in PO is set to Fine (1.25 mm) as default.
- The quality metrics Paddick CI, Paddick GI, ICRU83 HI (98%) and RTOG CI are available for all targets.
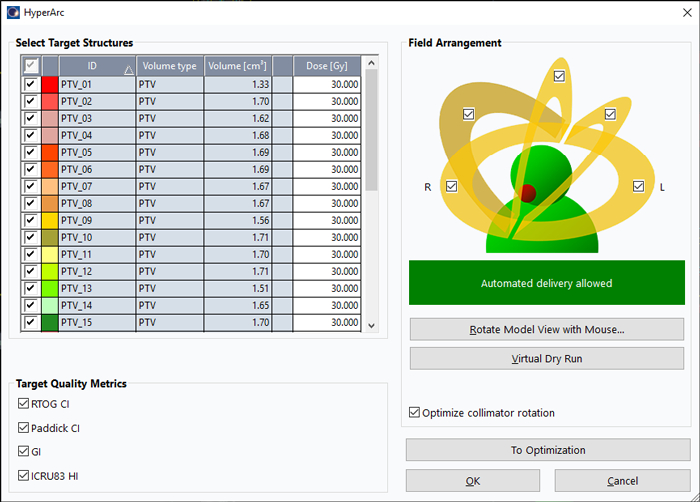
(The HyperArc dialog box at the beginning of the HyperArc planning workflow.)
The involved structures (PTVs) are usually small, and Varian has already taken some measures to reduce dosimetric inaccuracies which could arise from a mismatch between target size and the size of various grids3, as mentioned above. Documents exist which contain recommended settings for all parts of the workflow, starting with the imaging slice thickness of the planning CT.
On the TrueBeam, the workflow always starts with the mandatory 3D imaging (CBCT), followed by online matching and correction using the 6DoF PerfectPitch couch. The fully automated treatment is started by pressing beam on only once4.
Pushing the Limits - A Dose Planner's Nightmare?
Due to the large MLC leaf span in relation to brain size, there are practically no limits regarding the coverage of multiple targets using a single isocenter.
The simultaneous treatment of multiple brain metastases (BMs) is therefore the ideal application. Single targets can be treated as well, if the plan benefits from going non-coplanar. Total treatment time will not depend on the number and complexity of the targets, but rather on dose and the available dose rates.
What could easily become a Dose Planner's Nightmare (DPN) with certain treatment modalities (e.g. GammaKnife, CyberKnife), is a breeze in HyperArc.
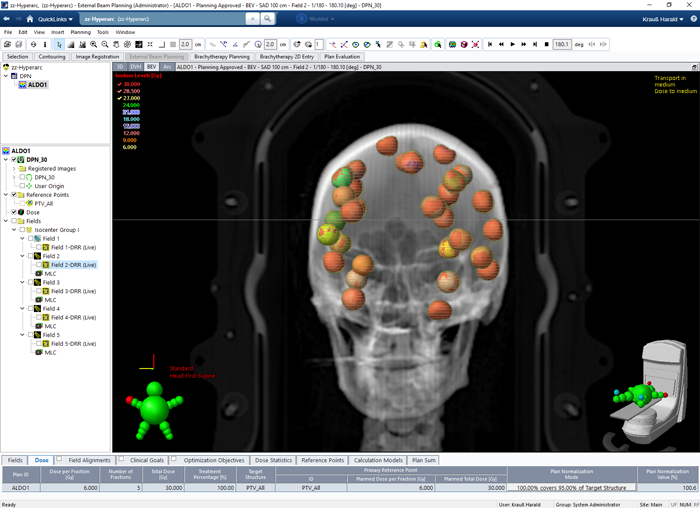
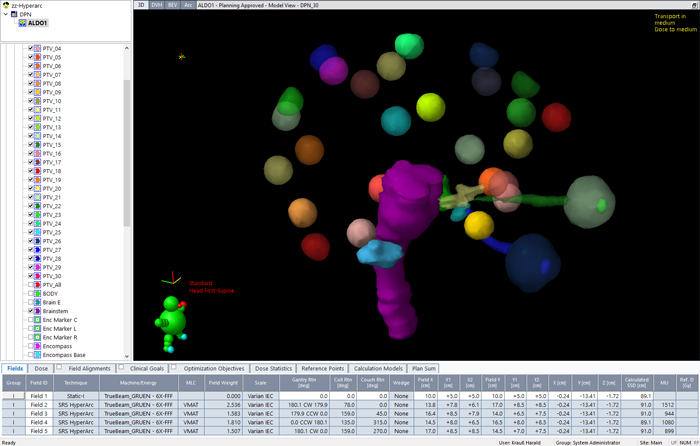
In the following example 30 targets, distributed on the inside of the skull, are optimized for testing purposes:
The targets have near-spherical volumes between 1.3 and 1.7 cm3. Dose prescription is 30 Gy in 5 fractions5.
Since this is a test which shall demonstrate HyperArc's capability of covering a large number of targets with a single isocenter, plan quality was not the top priority. OAR objectives were omitted. SRS NTO is so good that in many cases they are simply not necessary. Only if an OAR is in close proximity to a target, it may become necessary to add more objectives.
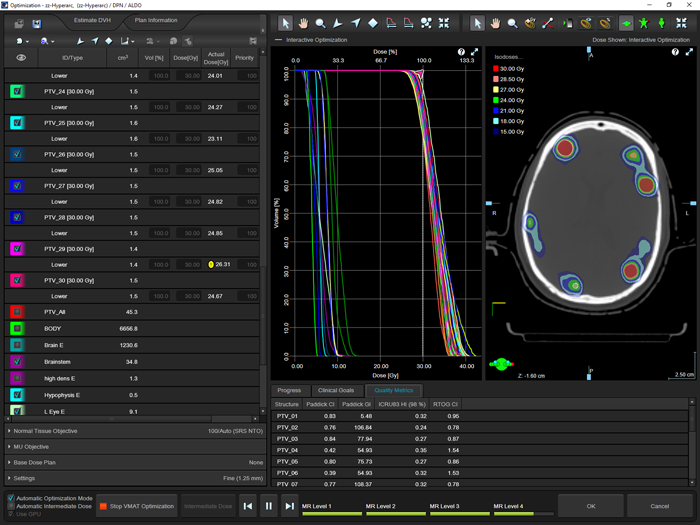
(During optimization with 30 targets.)
Optimization Timing
The time from start of VMAT optimization to display of the final 3D dose was 18 minutes. The following settings were used:
- Patient: 357 slices @ 1 mm slice thickness
- Photon Optimizer: Use GPU, structure resolution = fine, dose calculation resolution = high, convergence mode = OFF6, use ALDO, automatic intermediate dose with restart at level 4 (ALDO always restarts at this level)
- 3D dose calculation: Acuros XB (using GPU), calculation grid = 0.1 cm, full dose calculation matrix
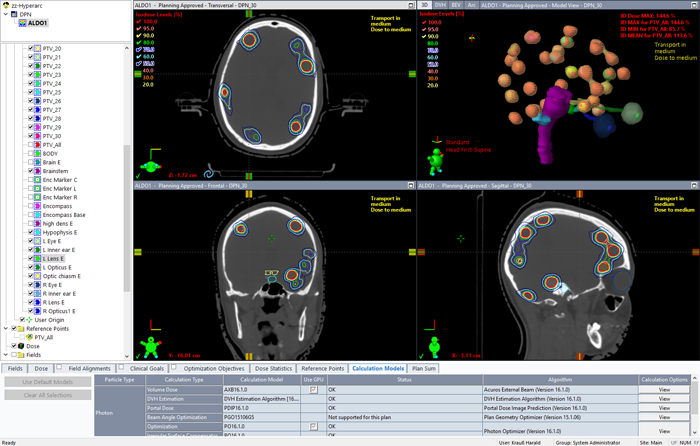
(The final dose distribution of the test plan.)
Leaf motions during the four arcs can be displayed in Beam's Eye View. The animation first displays solid leaves, and is repeated with transparent leaves:
Dosimetric Verification - A Physicist's Nightmare?
Even if the planning phase can be successfully completed (i.e., the DPN could be avoided), such plans can easily turn into a Physicist's Nightmare (PN) if pretreatment dose verification fails.
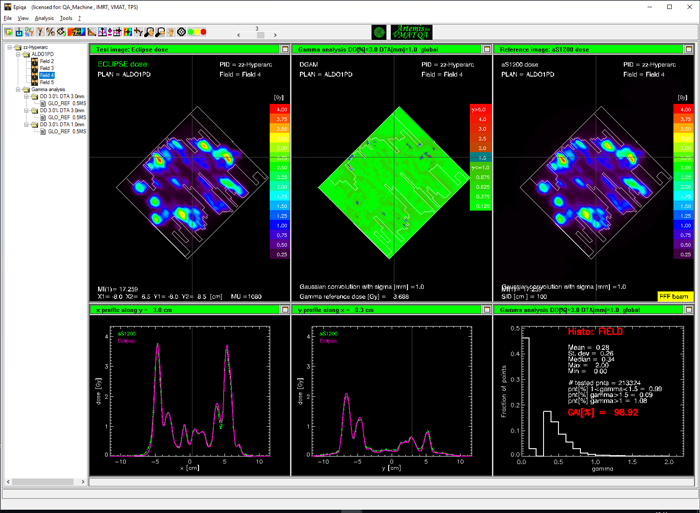
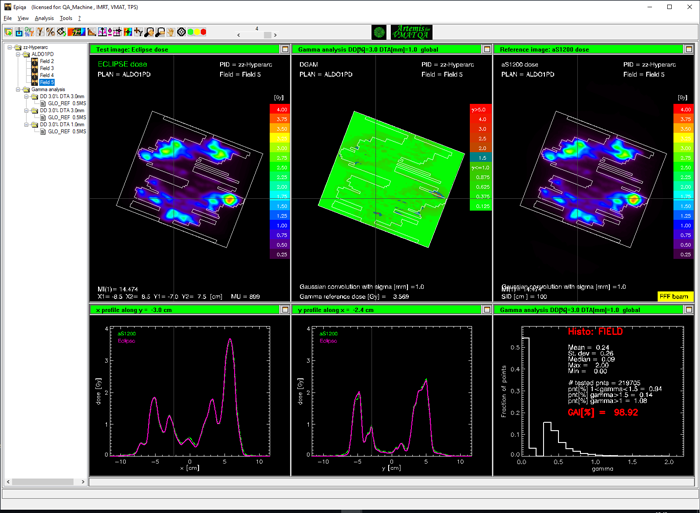
EPIQA, not Varian Portal Dosimetry (VPD), is our routine solution for pretreatment verification of HyperArc plans. In demanding cases, the advantages of EPIQA over VPD are simply striking.
Here we want to look into both, because we get the VPD results for free: the verification plan is a VPD plan anyway. After DICOM export, can be loaded in EPIQA. Additional items needed by EPIQA are the calculated dose matrices of each arc (Gantry collapsed), the delivered integrated images, and the measured 10x10 image.
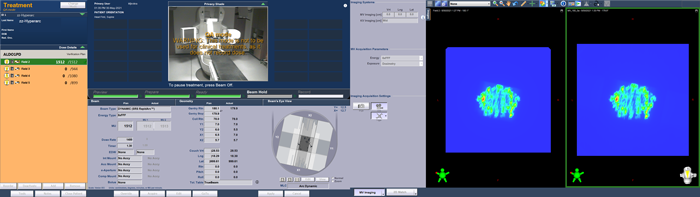
Delivery of the portal dosimetry plan on the TrueBeam took 4 minutes 18 seconds. Here are screenshots taken (approximately) at the beginning and end of each arc:
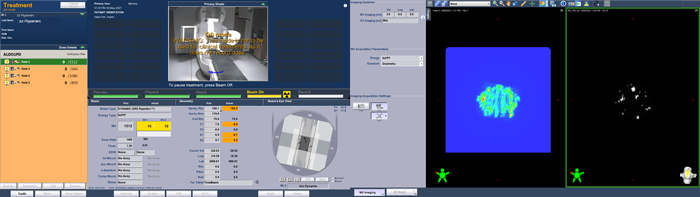
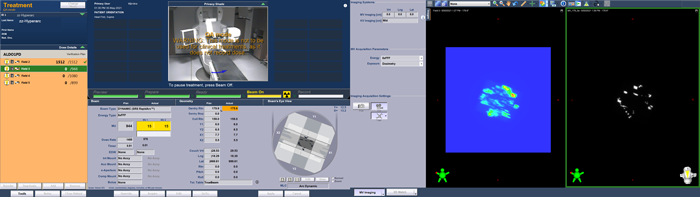
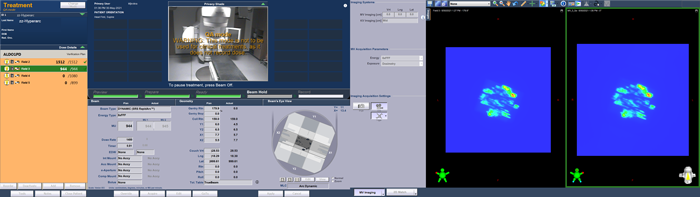

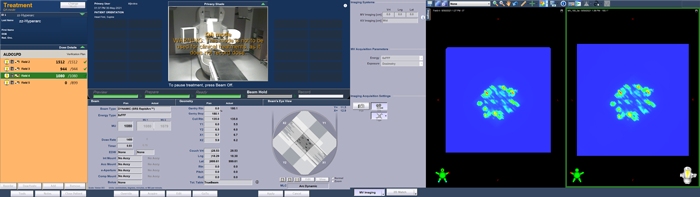
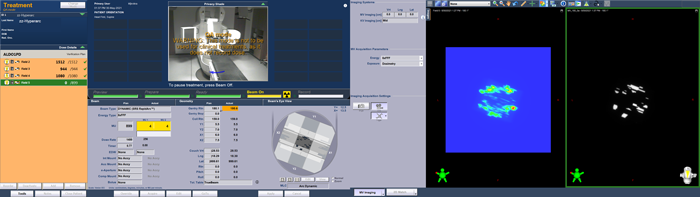
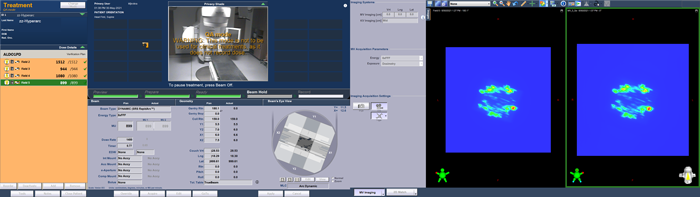 (The Portal Dosimetry plan is delivered in QA Mode.)
(The Portal Dosimetry plan is delivered in QA Mode.)
Due to MV imaging, it takes somewhat longer compared to a real patient treatment because the beam stops after each arc to present the integrated image. On the other hand, couch is not rotated in the portal dosimetry session.
It takes 4 minutes 43 seconds to deliver the 4435 MU of the plan in "clinical mode", i.e. including the automated couch rotations.
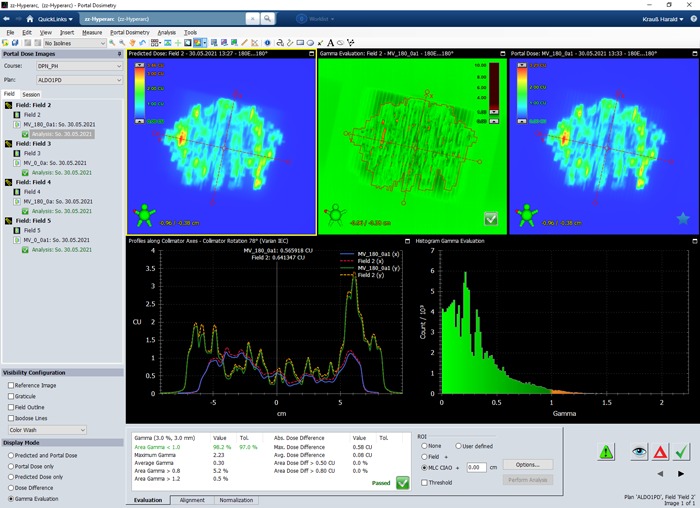
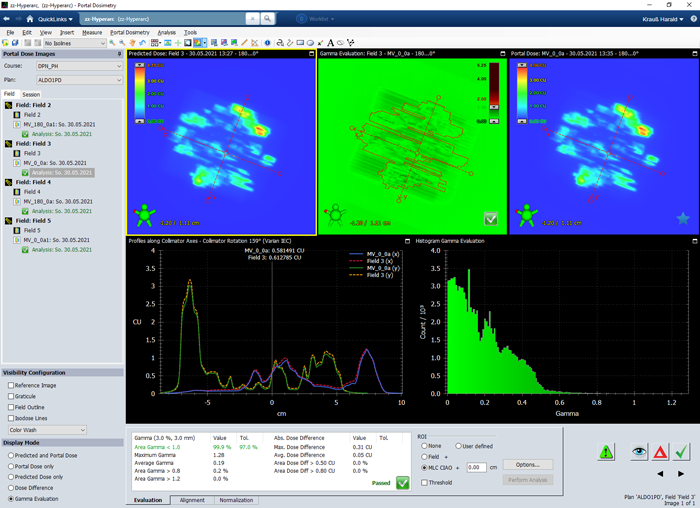
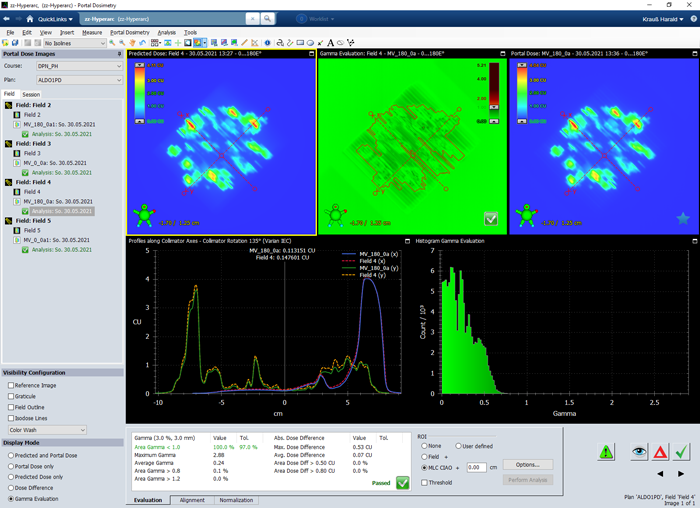
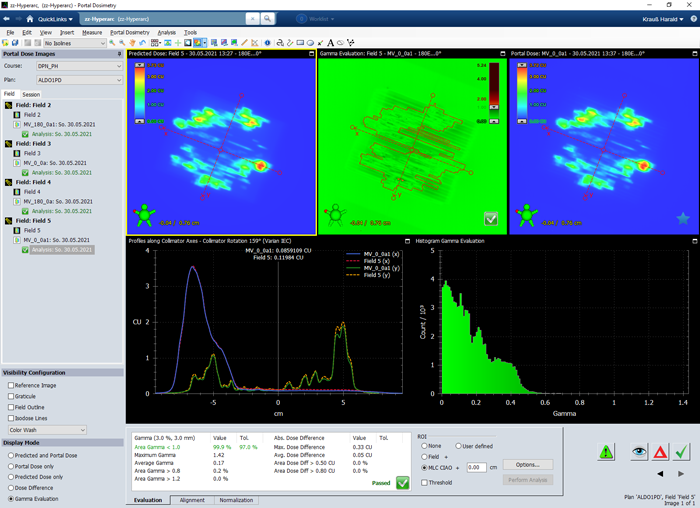
Results for Varian Portal Dosimetry
As can be guessed from the TrueBeam screenshots, the agreement between predicted (left) and measured (right) image is not so bad.
For normal (non-HyperArc) VMAT plans, we routinely use the 3%/3mm and 2%/2mm Gamma criterion, and evaluate the inside of the CIAO (Complete Irradiation Area Outline). A plan passes if the 3%/3mm passing rate is at least 97%.
If apply this to the HyperArc test plan, we get the following results for fields 2 to 5, respectively:
- VPD passing rates for Gamma 3%/3mm ("CIAO"): 98.2%, 99.9%, 100.00%, 99.9%.
In the 2%/2mm test (not shown), the first arc (Field 2) fails, because the passing rate drops to 91.0%.
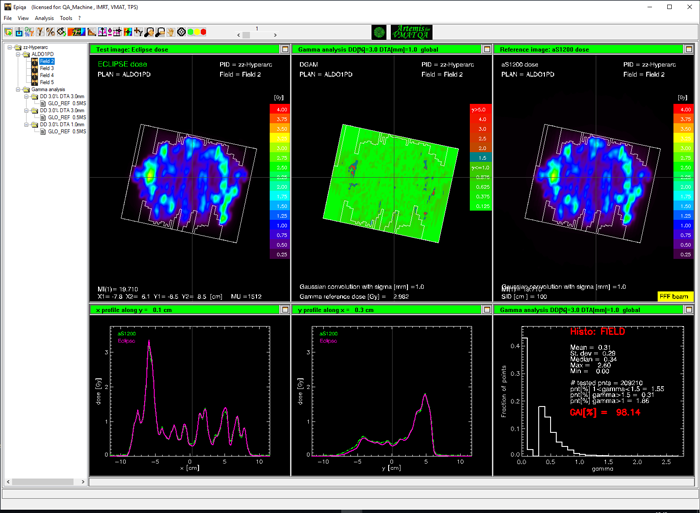
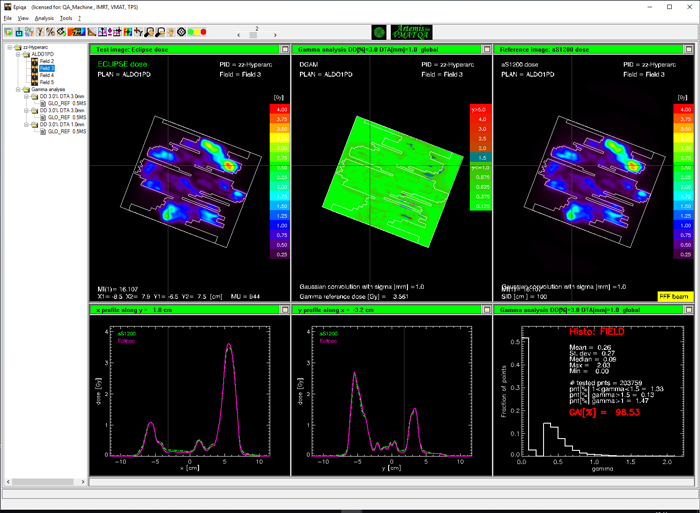
Results for EPIQA
We first evaluate the CIAO, and choose the 3%/3mm test as before:
Considering the high positioning accuracy of the TrueBeam mechanics (which is verified on a daily basis via MPC), one could ask for a more stringent DTA. We try 3%/1mm and keep the 97% tolerance level.
The HyperArc plan passes with flying colors:
- EPIQA passing rates for Gamma 3%/1mm ("Field"): 98.14%, 98.53%, 98.92%, 98.92%.
In the literature, one sometimes finds7 the criterion 2%/1mm in the context of stereotactic ablative radiotherapy, which is combined with evaluation thresholds of 5% or 10%. The tolerance level is relaxed to 90%.
Applying this criterion to the example plan gives the following results:
Removing the tolerance level gives slightly better passing rates:
Summary
HyperArc is an promising new treatment option for multiple lesions in the brain. The number of targets which can be adressed with one isocenter seems to be unlimited. In the example (energy: 6FFF, nominal dose rate: 1400 MU/min), 30 targets were treated simultaneously with 6 Gy. Delivery time for 4435 MU total was
- 4:18 minutes (QA session with MV imaging, no couch rotations), and
- 4:43 minutes ("clinical" delivery including automated couch rotations, no MV imaging).
With automation, single isocenter and FFF energies, treatment time is minimized. Spatial resolution is optimized by using the HD120 MLC with 2.5 mm leaf width at isocenter. Jaw tracking is ON per default, which optimizes dosimetry. Specialized algorithms (SRS NTO) reduce dose to healty tissue even more than standard algorithms.
Routine pre-treatment verification can be done either with Varian Portal Dosimetry or EPIQA. In the very demanding example, the plan passed an EPIQA Gamma test of 3%/1mm with passing rates beyond 98% for all arcs.
Neither DPNs nor PNs were triggered by this HyperArc example.
(Did we already mention that it can be fun to work with this equipment?)
Notes
1 In the animation, field numbering starts with Field 2. Field 1 is the imaging field (CBCT), which always comes first.
2 Objectives and priorities can be modified as required.
3 E.g., requirement for High Resolution Segments for all target structures, PO dose calculation resolution normal/high, PO structure resolution normal/fine, AAA or AXB calculation resolution in cm.
4 In the early phase and to gain confidence, semi-automatic treatments can be configured which acquire a single MV image before every arc and then stop. This gives the user the opportunity to check isocenter visually, do the match (2D2D) and even perform the shift, if necessary. However, semi-automation can not be configured on a plan-by-plan basis, only via TrueBeam System Administration.
5 This is a test case. Treating a real patient with this fractionation would have to be discussed.
6 If convergence mode is ON, the optimization takes somewhat longer because PO dwells longer in each multi-resolution (MR) level. Plan quality is generally better if convergence mode is ON.
7 "Kim, J, Chun, M, Wu, H, Chie, EKyu, Kim, HJae, Kim, JHo, & Park, JMin. "Gamma analysis with a gamma criterion of 2%/1 mm for stereotactic ablative radiotherapy delivered with volumetric modulated arc therapy technique: a single institution experience." Oncotarget 2017 Sep 29;8(44):76076-76084.